When patients arrive clutching two insurance cards, your billing team faces a critical task: determining primary vs secondary insurance coverage. Failing to identify which plan pays first risks resubmissions, delayed reimbursements, and frustrated patients. This guide delivers clear, step‑by‑step instructions free of jargon to help practices verify benefits, apply coordination protocols, and submit claims correctly the first time.
1. Why Getting Primary vs Secondary Insurance Coverage Right Makes a Difference
Healthcare revenue cycles hinge on accurate payer orders. Submitting to the wrong insurer first can trigger automatic denials, lengthy appeals, and cash‑flow gaps. By mastering primary vs secondary insurance coverage, your practice will:
- Reduce Denials
Accurate filing order slashes denials tied to coordination errors, meaning fewer claims bounce back for rework. - Accelerate Cash Flow
Billing the correct carrier first shortens days in accounts receivable, improving your bottom line. - Boost Patient Satisfaction
Clear, predictable billing builds trust. When claims process smoothly, patients see fewer surprise bills. - Ensure Compliance
Payer and state rules governing the coordination of benefits are non‑negotiable. Adhering to them protects your practice.
2. Defining Primary vs Secondary Insurance Coverage
At its core, primary vs secondary insurance coverage determines payment order:
- Primary Insurance Coverage is the plan you submit to first. The primary insurance carrier evaluates and pays claims up to its policy limits. This insurer handles deductibles, coinsurance, and copayments until those obligations are met.
- Secondary Insurance Coverage takes over after the primary insurer finalizes payment. The secondary payer covers remaining balances—deductibles, coinsurance, or non‑covered services—per policy terms.
Practices that correctly designate each plan avoid duplicate billing and ensure both payers fulfill their financial responsibilities.
3. The Difference Between Primary vs Secondary Insurance
Clinicians and billers alike often ask about the difference between primary and secondary insurance. In essence:
| Aspect | Primary Plan | Secondary Plan |
| Payment Order | First—processes claims up to policy limits | Second—covers leftover patient responsibility |
| Covered Costs | Deductibles, copays, and coinsurance according to plan specifics | Remaining balances after primary payment |
| Claim Submission | Standard CMS‑1500 or UB‑04 with patient details | Claim form plus primary Explanation of Benefits (EOB) |
| Patient Liability | Deductibles, coinsurance until limits are reached | Unpaid copays, coinsurance after primary payment |
| Denial Risk | Low when the information is complete | Higher if EOB is missing or coordination is misapplied |
By internalizing this table, your team will recognize when to bill each insurer and what to expect from each payment.
4. Coordination of Benefits Rules: Establishing Who Pays First
Accurate coordination of benefits rules ensures each plan pays its fair share. Though payers may have proprietary variations, four guiding principles apply across most states:
- Birthday Rule
If both parents have insurance, the one with the earlier birthday in the year is usually the primary coverage for the child. - Employment Status
An active employee’s plan generally takes priority over retiree, COBRA, or dependent plans. - Active vs. Retiree Coverage
Group health plans for active employees pay before Medicare for those still employed. Upon retirement, Medicare often becomes primary if no active employer coverage remains. - Medicare Coordination
Medicare is secondary if an active work health plan still covers you. It’s primary if you don’t have one.
Understanding and applying these rules reduces denials caused by payer disputes over coordination.
5. Step‑by‑Step Workflow for Dual‑Coverage Claims
A standardized workflow streamlines primary vs secondary insurance coverage management:
5.1. Front‑End Verification
- Collect Both Insurance Cards at scheduling and check‑in.
- Train staff on how to read a medical insurance card, ensuring they note subscriber names, group numbers, plan types, and coordination instructions.
5.2. Establish Payment Order
- Apply coordination of benefits rules based on subscriber status, employment, and Medicare eligibility.
- Enter both payers into your practice management system, designating primary and secondary fields accurately.
5.3. Submit to the Primary Insurer
- File the claim within the carrier’s timely‑filing window.
- Include required documentation such as referrals, prior authorizations, and clinical notes.
5.4. Review the Primary Explanation of Benefits
- Examine EOB details: paid amounts, adjustments, and patient responsibility.
- Identify any line‑item denials or services excluded.
5.5. File the Secondary Claim
- Attach the primary EOB to your secondary claim.
- Submit remaining balances for deductibles, coinsurance, or copays per policy terms.
5.6. Post Payments and Bill the Patient
- Once both insurers have processed, posted payments in your billing system.
- Issue a patient statement for any outstanding patient‑responsibility amounts.
Following this workflow ensures that neither insurer disputes payment order, and that patients only pay what they owe.
6. Common Pitfalls in Primary vs Secondary Insurance
Even well‑trained staff can encounter hurdles. Watch for these frequent mistakes:
- Incomplete Subscriber Information
Omitting birthdates, spelling errors, or wrong member IDs triggers denials. The institute double‑checks at intake. - EOB Misinterpretation
Misreading payment codes or adjustment reasons leads to billing errors. Provide regular training on common EOB layouts and codes. - Coordination Rule Errors
Flipping primary and secondary designations can result in immediate rejections. Maintain quick‑reference guides for coordination of benefits rules. - Missed Timely‑Filing Deadlines
Secondary carriers enforce their filing limits. Track primary EOB receipt dates and automate reminders for secondary submissions.
Addressing these pitfalls head‑on cuts denials and preserves revenue.
7. Leveraging Technology for Medical Insurance Coordination
Advances in practice management software have transformed medical insurance coordination:
- Real‑Time Eligibility checks automatically verify coverage and coordination rules before the visit.
- Dual‑Coverage Alerts flag when two active policies exist for a patient, prompting staff to confirm the payer order.
- Automated Secondary Claim Generation drafts and files claims once the primary EOB is received.
- Denial Analytics Dashboards identify patterns, such as denials for missing EOB attachments or late filings.
By embedding these tools, practices can reduce manual steps by up to 30%, accelerate payments, and focus on patient care rather than paperwork.
8. Best Practices for Smooth Coordination of Benefits
- Quarterly Staff Training
Refresh the team on the coordination of benefits rules and system updates. - Daily Claim Audits
Review claims flagged for dual coverage before transmission. - Robust Documentation
Maintain clear, organized records of all EOBs, authorizations, and payer communications. - Outsource Complex Billing
For specialized areas, like durable medical equipment, collaborate with a trusted DME billing company in San Diego, CA. Their expertise in supplier compliance and auditing frees your team to address core clinical tasks. - Performance Tracking
Monitor key metrics, first‑pass acceptance rates, secondary submission lag, and denial rates, to identify training gaps and refine processes.
These practices foster a culture of accuracy and accountability, ensuring your revenue cycle remains resilient.
9. Measuring Success: Key Performance Indicators
Tracking performance ensures continuous improvement in primary vs secondary insurance coverage management. Focus on these metrics:
- First‑Pass Acceptance Rate
The percentage of primary claims paid on initial submission. Target at least 90%. - Secondary Submission Lag
Days between primary EOB receipt and secondary claim filing. Aim for under five days. - Denial Rate for Coordination Errors: The proportion of denials linked to misfiled dual‑coverage claims. A rate below 2% indicates solid processes.
- Average Days in Accounts Receivable
Total days from service date to final payment. Strive for under 30 days for balanced cash flow.
Regularly reviewing these KPIs reveals trends, highlights root causes of denials, and offers clear insights on how to reduce billing errors through targeted staff coaching.
10. Real‑World Example: A Mid‑Size Practice Success Story
A mid‑size orthopedics group in Southern California faced relentless denials tied to dual coverage. By implementing this guide’s workflows—front‑end verification, precise coordination rules, and daily claim audits—they achieved:
- A 20% reduction in overall denials within three months.
- A drop in days in A/R from 45 to 28 days.
- Improved patient feedback, with complaints about surprise bills falling by 75%.
Their secret? Consistent application of primary vs secondary insurance coverage protocols and leveraging automated alerts for dual policies.
11. Staying Current with Coordination Rules
Payer policies and state regulations evolve. Maintain compliance by:
- Subscribing to major payers’ provider bulletins.
- Joining professional organizations focused on revenue cycle management.
- Attending webinars on updates to health insurance coordination of benefits.
Proactive education prevents surprises when carriers adjust their coordination guidelines.
12. Final Verdict
Managing primary vs secondary insurance coverage is fundamental to a healthy revenue cycle and positive patient experience. By:
- Verifying benefits and reading insurance cards accurately
- Applying coordination of benefits rules consistently
- Following a clear, step‑by‑step claims workflow
- Leveraging technology for eligibility checks and automated secondary filings
- Tracking performance metrics to drive continuous improvement
Your practice can dramatically reduce denials, accelerate cash flow, and keep patients happy. Implement these strategies today to transform complex billing into a competitive advantage and watch your financial performance soar.
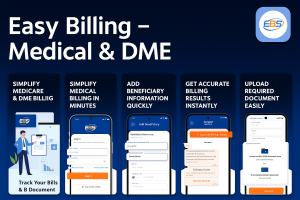
Precision in determining primary vs secondary insurance coverage can make or break your revenue cycle. Don’t let coordination mistakes stall your cash flow or burden your patients. Partner with Easy Billing Services LLC® today to:
- Eliminate dual‑coverage confusion.
- Slash denials tied to misfiled claims.
- Accelerate reimbursements.
Email us: info@easybillingservices.com
Call now: 877‑306‑2906
Frequently Asked Questions
What should be covered in contracts for billing services?
Contracts for medical billing services include the scope of work, performance metrics, data security, fees, and termination terms. Performance metrics, data security, fees, and termination terms.
What’s the core difference between primary vs secondary insurance coverage?
Primary pays first up to its limits; secondary covers remaining copays, coinsurance, and deductibles.
How do I know which plan is primary?
Use coordination rules, birthday rule, active‑employee status, and Medicare ordering, based on subscriber info at check‑in.
What must accompany a secondary claim?
Always attach the primary insurer’s explanation of Benefits (EOB).
How can I speed up durable medical equipment reimbursements?
Outsource to DME billing services in San Diego for specialized supplier compliance and faster payments.