Medicare billing guidelines are often difficult to navigate, but knowing the rules that matter is the key to simplifying claims and preventing compliance problems. Whether you are a healthcare provider, facility administrator, or billing professional, these seven important facts will assist in correct, timely reimbursement, and if you work with DME billing compliance services, being aware of certain compliance issues is also important for successful claims.

Medicare Billing Guidelines Compliance is Strictly Regulated
The Centers for Medicare & Medicaid Services (CMS) strictly emphasize that all claims must meet federal standards. Providers have to comply with documentation standards, correct coding efforts (CCI), and other compliance protocols to remain protected from denials and penalties. Keeping check of regulatory changes is vital to remain eligible for Medicare payment.
Lack of compliance could result in auditing, rejection of claims, and possible legal liabilities. Providers need to review CMS updates periodically, receive training on updates, and conduct internal auditing to align with Medicare billing guidelines at all times. Billing teams and compliance officers are supposed to remain close to put new regulations in place and follow a smooth process of billing.
In addition, Medicare has developed different integrity programs, including the Recovery Audit Contractor (RAC) program, with the intent of identifying and avoiding improper payments. Providers need to keep their records accurate and conduct self-audits in an effort to limit risks linked with compliance failure.
Proper Documentation is Essential for Claims Approval
Proper documentation ensures the medical need for services provided. Every claim should contain patient information relevant to the claim, physician referrals, and accompanying medical records. Medicare demands high documentation detail, and insufficiency in documentation may lead to denial or delay in reimbursement.
Aside from basic documentation, physicians must ensure on-time submission of documents, protected electronic storage, and an unobstructed audit trail to prove compliance with Medicare billing guidelines. The use of standardized templates for patient records facilitates enhanced consistency and accuracy in claims submission.
Providers must also be careful about Medicare’s “signature rules,” which contain specific regulations governing how and when a provider will sign medical records. Unsigned or, in certain cases, not properly signed records can result in claim denials.
Medicare Billing Guidelines Specify Specific Coding Systems
Medicare is based on the concept of CPT (Current Procedural Terminology), HCPCS (Healthcare Common Procedure Coding System), and ICD-10 (International Classification of Diseases) codes for processing a claim. Filling out these codes in the correct manner guarantees proper billing and avoids general coding mistakes which retard reimbursement.
Coding mistakes, like invalid procedure codes or misaligned diagnosis codes, will lead to audits or cause claim denial. Ongoing education on coding revisions, together with verification software, can aid providers in compliance with Medicare billing guidelines.
Medical necessity needs to be backed by proper codes. For example, an ICD-10 code should correspond accurately to the associated CPT code to support treatment. Automated coding systems or coding assistance with AI can enhance accuracy and reduce claim rejections.
Understanding Medicare’s Fee Schedule is Crucial
Medicare payments to providers are based on a fee schedule that varies by service type and geographic location. CMS adjusts annual reimbursement rates due to economic realities, policy development, and decisions by Congress.
Providers need to periodically review fee schedules to ensure proper billing and prevent underpayment or overpayment situations. Following outdated fee schedules could result in discrepancies in reimbursement that need costly corrections. Medicare also has a “limiting charge” provision, which prevents a non-participating provider from charging the patient more than the Medicare-set amount.
Familiarity with Medicare’s various payment systems, including the Resource-Based Relative Value Scale (RBRVS), can assist providers in optimizing reimbursement rates and managing financial planning in a better way.
Chiropractic Services Have Special Billing Requirements
Medicare covers chiropractic treatment under strict conditions. Medicare billing guidelines require specific codes to be applied for spinal adjustments, and only medically necessary therapy is covered. Maintenance therapy is typically not covered under Medicare.
Furthermore, chiropractors need to provide documentation that supports medical necessity, such as patient evaluations and progress reports. Failure to meet documentation guidelines may lead to the denial of claims or even possible audits. Chiropractors are advised to know Medicare’s Advance Beneficiary Notice (ABN) guidelines in the rendering of services that are not Medicare-covered.
Medicare will only reimburse chiropractic services if a patient has active spinal conditions that must be treated by manual manipulation. Providers must refrain from filing maintenance therapy claims because these claims are sure to be rejected.
DME Billing Requires Special Consideration
Separately billed durable medical equipment (DME) has to meet Medicare’s particular criteria for coverage. As a DME billing provider, prescriptions, documentation, and evidence of medical necessity need to be submitted in the right manner to prevent the denial of claims.
DME claims require physician orders, prior authorization where necessary, and delivery verification. Inadequate coding or failure to document delays payment and causes compliance audits. Medicare has put in place the Competitive Bidding Program (CBP) for DME suppliers in certain geographic areas, requiring certain suppliers to qualify on the basis of extra criteria prior to reimbursement.
Providers must check if the patient is eligible for DME coverage under Medicare Part B of Medicare billing guidelines and make sure that they are billing with the proper codes to correspond with the approved equipment categories. Electronic claim submission systems can also be employed to decrease errors and enhance processing efficiency.
Medicare Audits and Reviews Are Common
Medicare often audits providers’ claims to confirm compliance. Random and targeted audits evaluate if providers are compliant with Medicare billing guidelines. Maintaining precise records and using proper procedures decreases the risk of payment recoupment.
Audits can concentrate on medical necessity, coding, and billing trends. Providers are encouraged to maintain thorough documentation and prepare a response strategy to effectively deal with audit requests. The application of computer tracking systems for payments and claims submission can keep providers ahead of audit issues.
Providers under audit need to be ready to furnish requested documentation in a timely manner and coordinate with compliance officers to rectify any irregularities. Audit triggers, for instance, the excessive billing of certain services, can enable providers to take preventive action and correct anomalies before they snowball into serious problems.
Strategies to Improve Medicare Billing Success
In addition to knowing the basic Medicare billing guidelines, the providers may implement proactive measures to improve billing accuracy and compliance:
- Adopt Electronic Health Records (EHR) Systems: Computerized systems enhance documentation precision, verify appropriate coding, and simplify claim filing.
- Continuous Staff Training: Regular training for the billing personnel will keep them aware of the changing regulations and updates in codes.
- Internal Audits: Frequent examination of the billing procedure enables detection of likely errors and risk of non-compliance prior to an outside audit.
- Incorporate Billing Specialists: The hiring of expert billing professionals could guide providers through difficult regulations and help optimize payments.
- Utilize Claims Scrubbing Software: Such software assists in identifying errors prior to submission, lowering claim denials, and enhancing efficiency.
Final Thoughts
Being familiar with medicare billing guidelines ensures efficient claim processing and compliance. Providers who remain up-to-date and are in line with best practices lower denials and improve reimbursement chances. Through efficient billing practices and maintaining proper documentation, healthcare providers can make the most out of their Medicare reimbursements and avoid compliance problems.
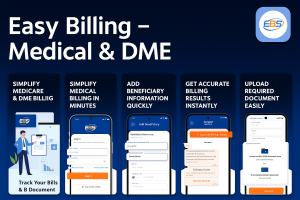
To obtain professional Medicare billing assistance and understand medicare billing guidelines, reach out to professionals like Easy Billing Services LLC®.
Call 877-306-2906 or send an email to info@easybillingservices.com for professional assistance.
Frequently Asked Questions
What is the purpose of medicare billing guidelines?
Medicare chiropractic billing guidelines help healthcare providers submit claims correctly to get proper reimbursements.
How can I avoid Medicare claim denials?
Submit complete and accurate documentation with proper codes and ensure medical necessity for all billed services to avoid rejection of claims.
What services require specific medicare billing guidelines?
Each specialty branch, including chiropractic care and durable medical equipment, needs to follow specific medicare billing guidelines.
Why is proper documentation important in medicare billing?
Medical records prove why services are needed and avoid payment issues.
What happens if I fail a medicare audit?
A medicare audit failure leads to the recoupment of payments along with financial penalties and may end your eligibility to receive Medicare payments.